Aim of STEMIcathAID Mobile App
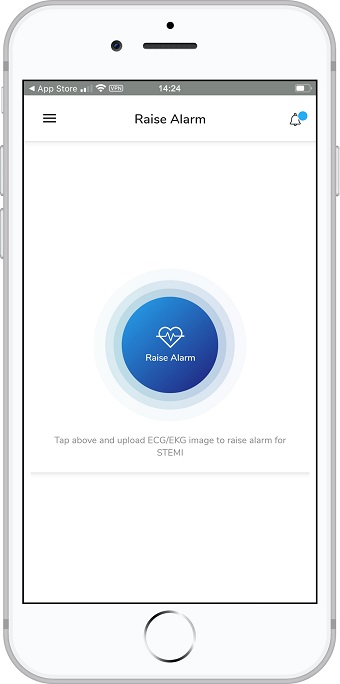
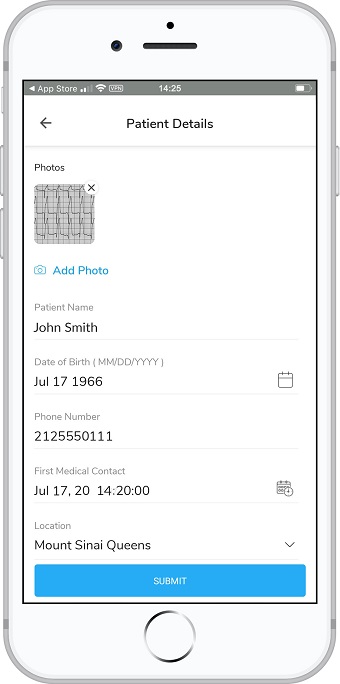
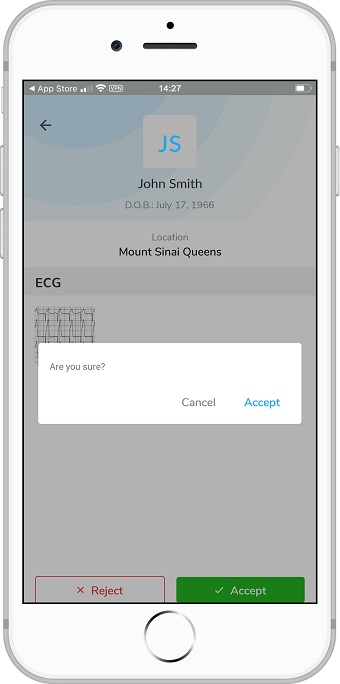
STEMI patient recognition, response, and record-keeping system designed to improve outcomes through adherence the American Heart Association’s Mission: Lifeline STEMI guidelines.
Early restoration of blood flow to occluded coronary vessels has been shown to significantly improve outcomes for high-risk STEMI patients. STEMIcathAID aims to improve these clinical outcomes by optimizing their treatment following many of the recommendations of the AHA by reducing the time to STEMI recognition, lead acquisition, STEMI identification, notification of the catheterization lab, and reperfusion.
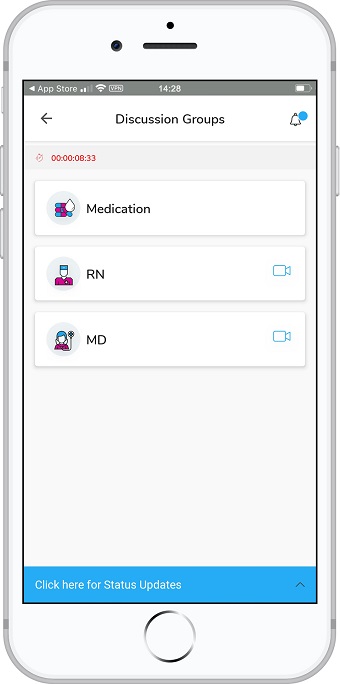
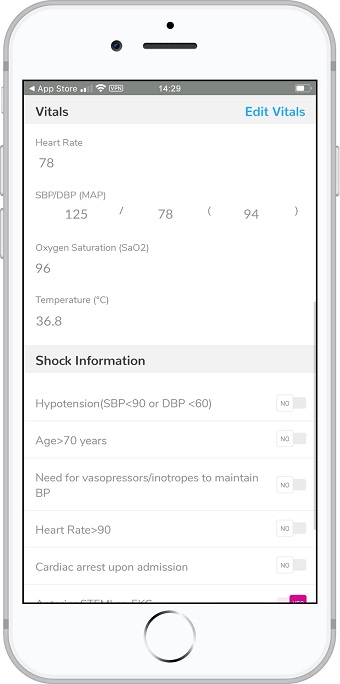
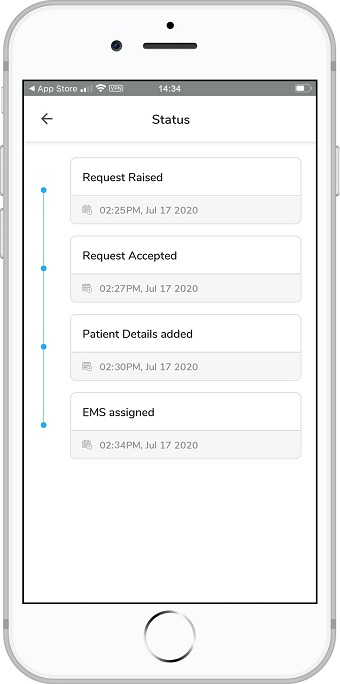
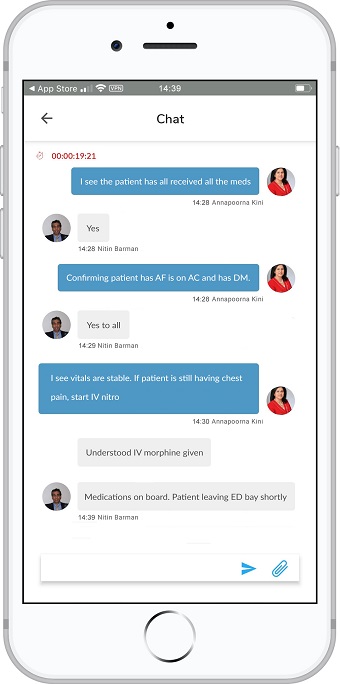
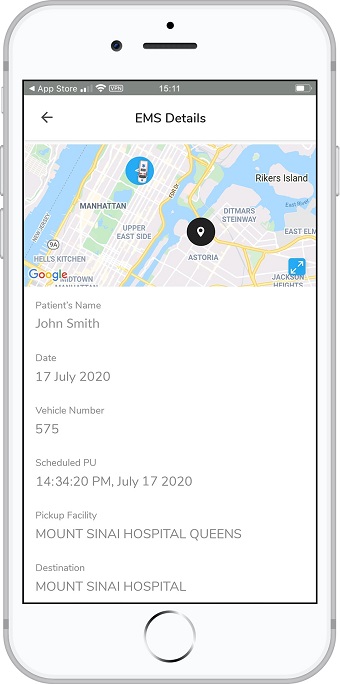
There are multiple personnel and steps involved in caring for these high-risk patients. STEMIcathAID takes an algorithmic approach which will enhance the coordination and communication tasks essential to rapid assessment and easy transfer of STEMI patients from the field or outside facility. It will also provide protocols for the EMS or outside hospital provider to identify patients in cardiogenic shock even before their arrival in the catheterization lab. The application will integrate live GPS tracking of the patients alongside the time the alarm was raised prompting the sense of urgency in transferring the patient.
If you have any additional questions, please do not hesitate to call 212-241-4452 or speak to someone from our experienced Mount Sinai Heart health care team. We are more than happy to answer any questions you may have.
We wish you a very positive experience at The Mount Sinai Hospital, a smooth recovery and a healthy future. Please feel free to contact us with any questions.